Blocking Cancer Cells from Spreading
Immune checkpoint blockade medications have revolutionized cancer treatment, giving patients and providers new hope to control and sometimes cure metastatic cancer. However, predicting which patients will benefit from this expensive and sometimes toxic, but potentially lifesaving, class of medications has been a challenge.
Now, UConn School of Medicine’s Dr. Margaret Callahan, chief of the Division of Hematology/Oncology at the Neag Comprehensive Cancer Center, and co-researchers show in Science Translational Medicine how a new mechanistic understanding of a specific immunotherapy combination may help guide future treatment decisions to match the right patient with the right therapy for them.
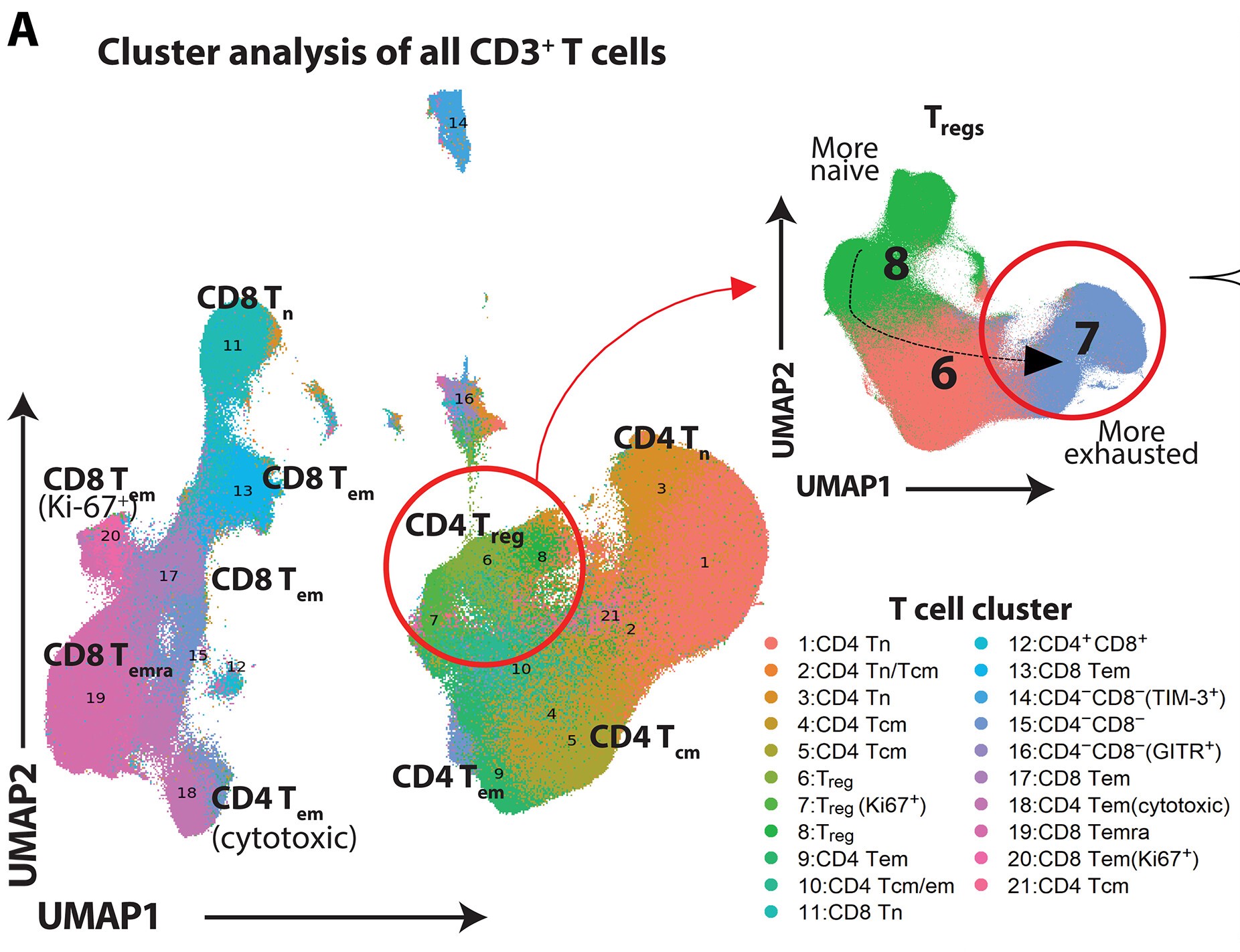
The research team first demonstrated that a combination of immune checkpoint-blocking antibodies, anti-PD-1 plus anti-LAG-3, can effectively influence a specific population of immune cells called regulatory T cells, known as Tregs, to make them less able to regulate the immune system. Then, a large clinical trial of metastatic melanoma patients receiving the drug combination of anti-PD-1 plus anti-LAG-3 also benefitted from the combination therapy and experienced the same changes in their Tregs.
Callahan says, “Together, our laboratory and human studies both show Tregs play a key, beneficial role for this drug combination and may serve as a biomarker to identify which patients will respond optimally.”
Latest UConn Today
- Building A World Where Young People Thrive: SSW’s Innovations Institute Hosts 2025 Training InstitutesThe UConn School of Social Work’s Innovations Institute offered more than 160 workshops focusing on ways to improve outcomes for children, young adults, and families
- Husky Reads Brings the Joy of Reading and Healthy Lifestyles to Connecticut PreschoolersThe UConn Husky Nutrition & Sport initiative connects UConn students with hundreds of young children across the state each year
- UConn Students Explore Entrepreneurship Across Borders Through an Abrahamic LensThe program will be offered again in Spring 2026
- Real Estate Professor Cohen: Study Confirms that Properties Adjacent to Tornado Destruction Initially Plunge in ValueLessons learned may apply to areas recovering from other natural disasters
- Elite Neurosurgery Residency Thriving at UConnMeet one of the future neurosurgeons training at UConn, Dr. Taylor Burch. As a Black woman, she’s a rarity in the neurosurgery field
- Carolan Awarded NIH Loan Repayment Award in Recognition of her Long-COVID ResearchKelsi Carolan, assistant professor in UConn’s School of Social Work, is investigating the effects of long-COVID on employment, family and social relationships, and mental health